
Optimal Health for Frail Older Adults:
Best Practices Along the Continuum of Care
A resource produced by the
Committee on Clinical and Scientific Affairs
Ottawa, ON
July 2009
2
Table of Contents
Acknowledgements Page 4
Introduction Page 5
Best Practices for Aging Adults in Private Dental Practice Page 6
The Aging Population Page 6
The Importance of Prevention Page 6
Rational Dental Care for the Elderly Page 7
Medical Issues Page 8
Palliative Dental Care Page 10
Educational Resources Page 11
References Page 11
Best Practices for Dental Care for the Homebound Page 13
Best Practices for Oral Care in Long-Term Care (LTC) Facilities Page 13
Organizational Support Page 13
Multidisciplinary Approach Page 13
Facility Policy for Oral Care Page 13
Assessment Page 14
Oral History on Admission Page 14
Regular Oral Assessment Page 14
Oral Care Plan Page 14
Education of Staff Page 15
Resources Page 15
Appendix A: Community Form Patient Information Record Page 17
Appendix B: Hospital Facility Patient Information Record Page 18
3
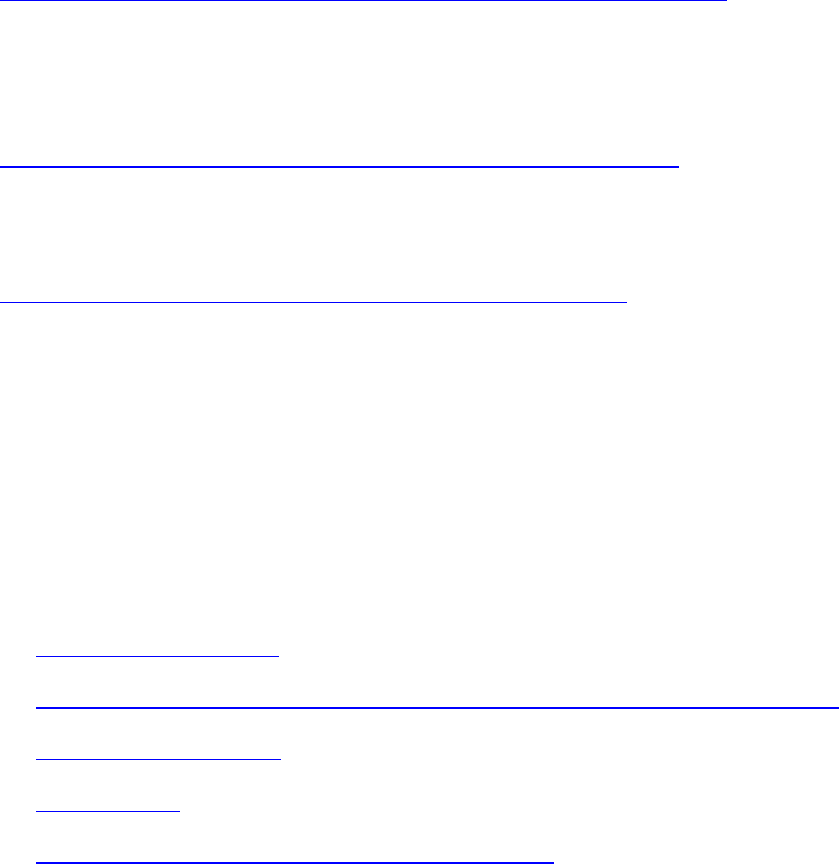
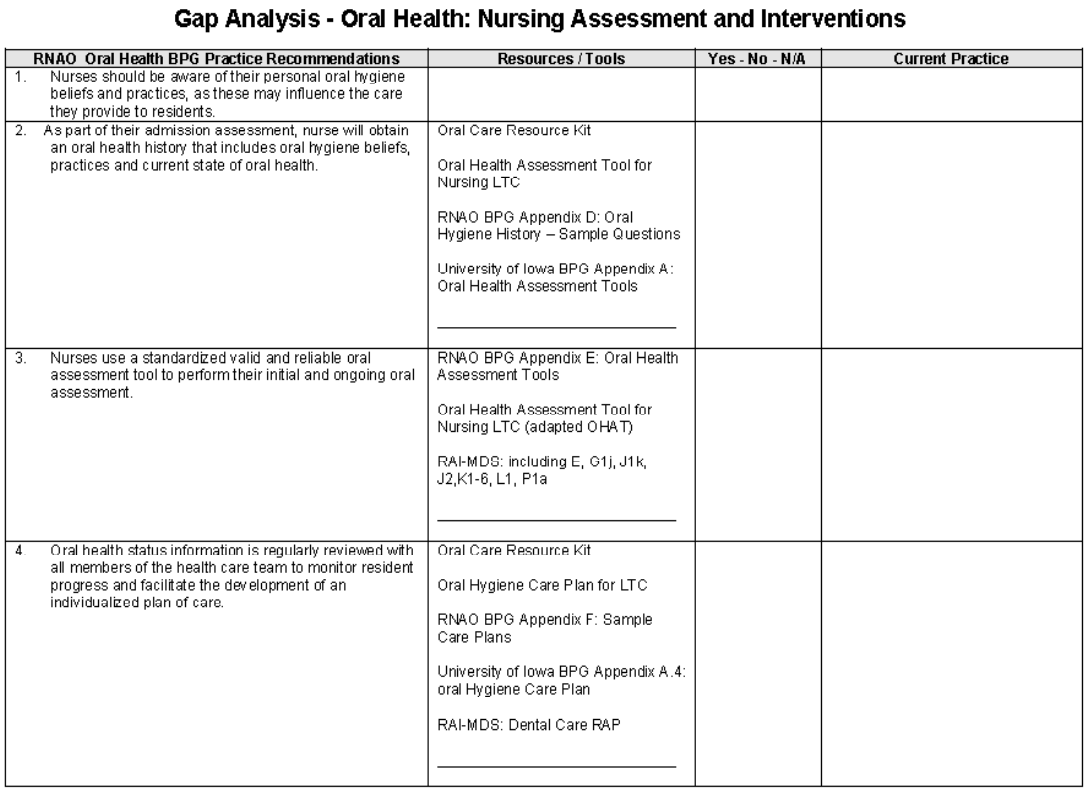
Appendix C: Oral Care Gap Analysis Page 19
Appendix D: Sample LTC Oral Care Policy Page 22
Appendix E: Sample Oral Hygiene History Page 26

4
Acknowledgements
The CDA’s Committee on Clinical and Scientific Affairs acknowledges the resources and
information available on the public websites of the following organizations:
American Dental Association www.ada.org
British Society for Disability and Oral Health www.bsdh.org.uk
Halton Region Health Department – Dental Health (Ontario) www.halton.ca
Regional Geriatric Program central (Ontario) www.rgpc.ca
Registered Nurses’ Association of Ontario www.rnao.org
University of British Columbia ELDERS Group www.elders.dentistry.ubc.ca
University of Manitoba’s Centre for Community Oral Health www.umanitoba.ca/dentistry/ccoh
5
Optimal Oral Health for Frail Older Adults:
Best Practices Along the Continuum of Care
INTRODUCTION
The Canadian Dental Association recognizes that oral health is directly linked to general health.
Older adults with complex health conditions are at greater risk for oral diseases, which can have a
profound impact on chewing, swallowing and nutrition; increase susceptibility to systemic
infectious diseases, especially pneumonia; cause pain; and affect quality of life issues such as self-
image, communication and social interaction. As elderly persons become more frail and dependent,
with increasing medical comorbidities, multiple medications, physical and/or cognitive
impairments, and require greater dependence on caregiver support, the risk for oral diseases
increases and the negative effect on general health and well-being accelerates.
Best dental and oral care practices for seniors are needed along the continuum of care, as more
seniors and government health agencies embrace an “aging at home” strategy. For aging patients in
private dental practice, a common sense or rational approach to oral health care may facilitate their
oral care and provide for better oral health in later stages of life, when they are partially or fully
dependent on others for daily personal care. Patients who are homebound and cannot attend the
dental office may have an increased need for care, yet do not have the level of assistance provided
in the long-term care setting. As for seniors residing in long-term care facilities, they are a diverse
group that requires initial and ongoing assessment as well as individual care plans based on
accepted best care practices. End-of-life or palliative oral care best practices may apply to patients
in any of these three settings.
The philosophy of rational provision of oral health services for the elderly extends across the
continuum of care, with care plans modified based on the unique circumstances of an individual
patient. Some of the resources provided in the section on long-term care may be equally useful in
private practice and home settings. For all patients, but especially elderly patients, an
interprofessional approach to care is important, with sharing of information and expertise among
dental providers, physicians, nurses, pharmacists, dieticians, social workers and others.
Access to care is an essential component of ensuring optimal oral health for frail older adults.
Canadians of all ages value fair and equal access to health care as a basic right. The Canadian
Dental Association supports this right. This resource was created to help ensure that the elderly
continue to have access to care, regardless of their health and living conditions. Inadequate oral
health care can have far-reaching consequences. It is important that oral care be viewed within the
broader context of health care, and that all care providers work together to promote and ensure the
general health and well-being of our aging population.
6
BEST PRACTICES FOR AGING ADULTS IN PRIVATE DENTAL PRACTICE
1. The Aging Population
• The population aged 65 years or older is significant (13%) and increasing. This group of
aging adults is a diverse and heterogeneous population with varying dental needs, medical
conditions and behavioural characteristics. Approximately 95% of people over the age of 65
live in the community. Of these, 5% are homebound and 17% have mobility limitations.
Over 70% can therefore still travel to a dentist. (Ettinger 2006)
• The majority of older adults are relatively healthy and mobile. These “independent older
adults” have treatment requirements no different from other adult patients. However, when
treating this population, the dentist should be cognizant of approaching older age, the
development of associated health issues (e.g., medical problems, use of more medications,
reduced dexterity, social issues) and increasing oral disease as older patients become more
frail, more dependent and more cognitively impaired. (Chalmers 2006a) Many frail older
adults still attend private dental practices but may require special transport and/or be
accompanied by a caregiver.
• Currently, no definitive, published, evidence-based clinical guidelines are available for this
aspect of dental practice. However, many useful articles and special reviews on the medical
and dental problems facing this population of patients provide advice on appropriate care
management.
2. The Importance of Prevention
• Changing and increasing caries patterns in aging dentate patients have created more
challenges for clinicians. Development of rampant caries is possible even while patients are
still living in the community. (Chalmers 2006a) As people live longer and retain more teeth
that are often already heavily restored, they will require significantly more complex
treatment.
• While the older dentate patient is still relatively healthy, considerable emphasis should be
placed on caries prevention education. This should be designed to ensure sound preventive
habits are established before problems develop and should include information on oral
disease, the importance of an appropriate diet (minimal consumption of fermentable dietary
sugars and carbohydrates, particularly between meals), patient-specific oral hygiene
methods and techniques, and the prescription of additional patient-specific measures to
increase tooth resistance (e.g., in-office fluoride varnish, home fluoride rinses or
chlorhexidine). A good preventive regime for the relatively independent older adult with
7
increasing caries risk involves 3 weeks use of 0.2% fluoride rinse nightly, alternating with 1
week of 0.12% chlorhexidine used twice daily. (Featherstone et al. 2003) In-office caries
prevention could also include the regular use of direct application of fluoride varnish on
teeth at risk. Sugar substitutes, particularly the use of xylitol (non-acidogenic) chewing gum,
can be effective.
• As elderly patients grow more frail, managing their oral care becomes more complex and
challenging, and treatment possibilities will depend on a number of modifying factors.
(Lindquist and Ettinger 2003)
3. Rational Dental Care for the Elderly
• The four key areas of dental need to be considered when treating frail elderly are function,
symptoms, pathology and esthetics. (Berkey et al. 1996) These areas will require pragmatic
modification based on fundamental issues such as illness and degree of functional and
cognitive impairment.
• The concept of “rational care” for medically compromised elderly patients, which can be
more appropriate than “technically idealized care”, was introduced in 1984. (Ettinger
1984) A key issue in rational dental care is the understanding of what is an acceptable oral
status for a particular patient, as opposed to a subjective estimate of need based on the
dentist’s own experience.
• “Oral impairment and disability are inevitable features of old age, but they do not
necessarily have a negative impact on one’s quality of life.” (MacEntee 2007)
• Rational dental care involves “individualized care with all modifying factors evaluated and
considered” (Ettinger 2006). Factors include the patient’s ability to tolerate the stress of
treatment, the possibility of reasonable and less extensive treatment alternatives, how the
patient’s dental problems affect his or her quality of life, as well as the patient’s ability to
maintain oral health independently. The idea that “nothing less than idealized dentistry is
secondhand, compromised care offered by bad dentists” has been strongly refuted.
• Treatment for the “biologically compromised” older dental patient should ideally take place
in shorter appointments in a comfortable, supportive and positive environment with capable
practitioners. Treatment plans may need to evolve over time as treatment progresses and the
patient’s situation changes. (Lindquist and Ettinger 2003)
• Caries in frail older patients or patients with early dementia may often need to be managed
by conventional hand instruments and a slow-speed handpiece. For anterior esthetic
8
restorations where moisture control is possible, a composite resin, glass ionomer or glass
ionomer/composite sandwich technique is appropriate. Where moisture control is less than
optimal, the material of choice will be glass ionomer — or even a temporary zinc oxide and
eugenol material. For posterior restorations where moisture control is less than optimal, the
material of choice will be amalgam or glass ionomer, especially for subgingival locations.
(Chalmers 2006b) Long-term temporary restorations using hard-setting zinc oxide and
eugenol can also be extremely useful in difficult management situations. Fractured teeth can
be maintained simply by smoothing any sharp edges to ensure patient comfort.
• For deep caries there is increasing evidence that the deepest layers of carious dentin in a
vital tooth may not require removal, or may be treated successfully through two-stage
(stepwise) restorative management. (Van Thompson et al. 2008) Although management of a
deep carious lesion would normally involve two-stage treatment using a temporary
restorative material, an expedient, safe and pragmatic technique for the biologically
compromised older patient is to place a permanent restorative material at the first visit,
leaving deeper caries in appropriate situations (Chalmers 2006b) Avoiding exposure of the
carious pulp will reduce the need for more invasive treatment such as endodontic therapy or
extraction.
• The rate of total edentulism has steadily decreased over the past 50 years due to a
combination of improved access to dental care, diet and prevention. However, the rate of
partial edentulism has increased, especially in the elderly. The demand for dental prostheses
to replace missing teeth is significant. For healthy older adults, fixed or removable partial
dentures or implant-supported crowns may be considered. For patients missing a limited
number of posterior teeth, especially a single posterior unit, the best option is often no
treatment. A shortened dental arch limited to a combination of two opposing bicuspids
and/or molars per side provides adequate function at any age. When considering tooth
replacement for frail older adults, the least intrusive and most cost-effective means should
be considered. A well-designed and constructed acrylic removable partial denture is often
the best solution. This prosthesis will require relining over time to compensate for residual
ridge resorption, but has the advantage of easy conversion to a complete denture if the
remaining teeth are lost. All dental prostheses require reassessment and maintenance over
time; the removable partial denture in particular tends to collect plaque on surfaces in
contact with teeth, making these teeth more susceptible to caries and gingivitis.
4. Medical Issues
Systemic diseases are more common in older adults, even among those who are functionally
independent. Dental professionals need to be aware of the medical status of older patients, the
medications they are taking and the possible effects of these drugs on treatment. Before the first

9
appointment, and every recall appointment thereafter, it is advisable to ask older patients or their
caregiver to bring a printed list of medications and dosages. A standardized referral form or
patient information form received before the first visit to the dental office may be helpful. Two
examples of patient information forms are available for use in Appendices A and B. These
documents can also be found in Word and PDF format on the CDA website at http://www.cda-
adc.ca/en/dental_profession/practising/best_practices_seniors/default.asp. The first appointment for an
elderly patient should be of sufficient length to allow for an unhurried medical history and oral
examination.
• Older people tend to be more sensitive to drugs and to invasive dental treatments. Dentists
should use local anesthesia whenever possible as the risks of general anesthesia are greater
in older patients than in younger patients. Local anesthetic used with recommended dosages
of epinephrine has no significant effect on cardiac arrhythmias in functionally independent
older patients. (Scully and Ettinger 2007)
• The 10 most common systemic diseases found in the aging population that influence oral
health care have been described by Scully and Ettinger (2007):
o Arthritis (reduced dexterity for oral hygiene, joint discomfort in the dental chair,
tendency to bleed, possible need for corticosteroid supplementation and antibiotic
coverage for joint prostheses).
o Head and neck cancer (need for oral health before cancer therapy, reduced salivary
flow after radiotherapy, management of oral ulceration, mucositis and candidiasis).
o Chronic obstructive pulmonary disease (management depends on extent of
dyspnea, medications include bronchodilators and/or corticosteroids, patient best
treated upright).
o Diabetes (risk of hypoglycemia is main concern during dental treatment, well-
controlled diabetics tolerate procedures well, poorly controlled will require referral
for invasive procedures; diabetics may be immunocompromised, more susceptible to
infections and may require more aggressive infection management).
o Ischemic heart disease (training in CPR and emergency procedures necessary, level
of stability of disease important, stress-reduction protocols, limiting of epinephrine,
knowledge of INR).
o Hypertension (control before treatment, avoidance of anxiety and pain).
10
o Mental health, cognitive impairment, Alzheimer disease (behavioural problems,
adverse drug reactions, increased oral disease, reduced cooperation as disease
advances).
o Osteoporosis (fractures, bisphosphonates).
o Parkinson disease (involuntary movements, COMT inhibitors may interact with
epinephrine, restorative care increasingly difficult).
o Stroke (confusion, mobility and/or communication problems, deterioration of oral
hygiene, defer elective care for 3 months, short sessions, treat patient upright).
The authors conclude that the dentist’s focus should always be on prevention of dental
disease, especially in people who have progressive debilitating systemic diseases.
• Saliva flow rate may be reduced in elderly people due to medications and various associated
medical conditions. Xerostomia (dry mouth) is the most common adverse drug-related
effect in the oral cavity and has been associated with over 500 medications. It is common in
patients being treated for hypertension or mental illness. Because of the synergistic effects
of multiple medications, dry mouth is a particularly common and significant problem for
elderly patients. (Porter et al. 2004) Lack of saliva often causes soreness, dryness of the
mucosa and lips, caries, candidiasis and intolerance to removable dentures. An increase in
the severity of xerostomia can lead to a greater risk of dysphagia, choking and nutritional
problems. (Madinier et al. 2009) Management includes general and local hydration, saliva
substitutes and lubricants, local agents to stimulate secretion (e.g. sugarless gum), antifungal
treatment, modification of the diet and nutritional supplementation. (Madinier et al. 2009)
Intense caries prevention is essential. Dialogue with the patient’s physician is recommended.
5. Palliative Dental Care
• For the frail, elderly, dependent adult still in the community and attending private dental
offices with a caregiver, the concept of palliative dental care is appropriate — particularly if
the patient has dementia. In such cases, care involves “regular hygiene to reduce bacterial
invasion of the lungs, relief of pain and ‘maintenance of dignity’.” (MacEntee, private
correspondence)
• Focusing on idealized dental care for the frail older patient with a failing dentition, without
recognizing the stress and expense involved and without taking into account the limited
therapeutic benefits, can exaggerate the need for treatment (MacEntee 2007) and lead to
pointless and unnecessary over-treatment.

11
• The average length of stay in a long-term care residence depends on the gender and age of
the resident, as well as the level of care required. Eighty-five percent of nursing home
residents are 75 years of age or older. The average expected length of stay for this age group
(for all levels of care) averages 3.9 to 4.5 years across regions of Manitoba. (DeCoster et al.
1995) Individuals needing lower levels of care stay, on average, much longer than
individuals needing higher levels. The average length of stay for Veterans Affairs Canada’s
in-patients in long-term care facilities (average age over 80 years) was less than 1.9 years for
2005-06. (Veterans Affairs Canada data, Dec 2006)
• The goal of palliative care for seniors who are either terminally ill or approaching the end
stage of life is not to focus on disease, but rather on quality of life and the relief of
discomfort and pain. Early identification and rational management of potential dental
problems play an important role in relieving suffering at this stage of life.
6. Educational Resources
As part of its Oral Longevity initiative, the American Dental Association has developed
educational resources to assist dentists in educating patients, consumers and health
professionals about oral care for the elderly.
7. References
Berkey DB, Berg RG, Ettinger RL, Mersal A, Mann J. The old-old dental patient: the
challenge of clinical decision-making. JADA 1996; 127:321-332.
Chalmers JM. Minimal intervention dentistry: part 1. Strategies for addressing the new
caries challenge in older patients. J Can Dent Assoc 2006a; 72(5):427-433.
Chalmers JM. Minimal intervention dentistry: part 2. Strategies for addressing restorative
challenges in older patients. J Can Dent Assoc 2006b; 72(5):435-440.
DeCoster C, Roos NP, Bogdanovic B. Utilization of nursing home resources. Medical Care
1995; 33(12):DS79-82.
Ettinger RL. Rational dental care: part 1. Has the concept changed in 20 years? J Can Dent
Assoc 2006; 72(5):441-445.
Ettinger RL. Clinical decision-making in the dental treatment of the elderly. Gerontology
1984; 3:157-165.
12
Featherstone JD, Adair SM, Anderson MH, Berkowitz RJ, Bird WF, Crall JJ, Den Besten
PK, Donly KJ, Glassman P, Milgrom P, Roth JR, Snow R, Stewart RE. Caries management
by risk assessment: consensus statement, April 2002. J Calif Dent Assoc 2003; 31(3):257-
69.
Friedlander AH, Norman DC, Mahler ME, Norman KM, Yagiela JA. Alzheimer’s disease:
psychopathology, medical management and dental implications. JADA 2006; 137:1240-
1251.
Lindquist TJ, Ettinger RL. The complexities involved with managing the care of an elderly
patient. JADA 2003; 134:593-600.
MacEntee MI. Quality of life as an indicator of oral health in older people. JADA 2007;
138:47S-52S.
Madinier I, Starita-Geribaldi M, Berthier F, Pesci-Bardon C, Brocker P. Detection of mild
hyposalivation in elderly people based on the chewing time of specifically designed disc
tests: Diagnostic accuracy. J Am Geriatr Soc 2009; 57:691-696.
Porter SR, Scully C, Hegarty AM. An update of the etiology and management of
xerostomia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004; 97:28-46.
Scully C, Ettinger RL. The influence of systemic diseases on oral health care in older adults.
JADA 2007; 138:7S-14S.
Van Thompson, Craig RG, Curro FA, Green WS, Ship JA. Treatment of deep carious
lesions by complete excavation or partial removal. A critical review. JADA 2008; 139:705-
711.

13
BEST PRACTICES FOR DENTAL CARE FOR THE HOMEBOUND
Dentists may want to visit patients in their own home, or may be called to do so. The British Society
for Disability and Oral Health has developed guidelines for the provision of at-home oral health
services for homebound patients. This resource offers practical advice about offering care in the
home setting environment, including infection control and other safety issues, and the planning and
provision of treatment.
BEST PRACTICES FOR ORAL CARE IN LONG- TERM CARE (LTC) FACILITIES
1. Organizational Support
For an oral health care program to be successful, there needs to be support at all levels within
the facility and a culture that values and promotes oral health as a basic right of residents that is
integral to their overall health and well-being. Champions within the facility should be
identified to oversee the program and liaise with all members of the team. As part of the
organization’s quality assurance program, the facility should monitor and evaluate its oral care
program and ensure its sustainability.
2. Multidisciplinary Approach
An interprofessional approach should be used for the design, implementation and evaluation of
the oral health care program. LTC administrators and champions should contact local dental
organizations to develop partnerships and for assistance in identifying dental professionals who
can work as part of the program team. Provincial associations and/or local dental societies
should identify facilities and health networks within their area to develop partnerships and
promote interprofessional capacity to support oral care programs in LTC facilities.
3. Facility Policy for Oral Care
All LTC facilities should develop policies regarding oral health best practices. New or existing
policies and procedures should be evaluated, so that gaps between current and best practices can
be identified and corrected. Ontario’s Regional Geriatric Program central (RGPc) has developed
a resource that facilitates the comparison of an LTC facility’s practices, policies and procedures
to those in the Registered Nurses Association of Ontario (RNAO) Oral Health Best Practice
Guideline (see Appendix C). A sample oral care policy for LTC facilities is included with this
document (see Appendix D).

14
4. Assessment
Entry into an LTC facility provides an opportunity for a thorough oral assessment of the patient,
identification of oral problems that require attention, and ongoing nursing assessment and oral
care. A dental examination or an oral assessment by a qualified dental health professional
should be completed or arranged shortly after admission and periodically thereafter. These
examinations should be supplemented by oral health assessments and screenings by nurses and
caregivers, as outlined below.
4.1. Oral History on Admission
Within 24 hours of admission, an oral health history should be taken in addition to the
Minimum Data Set (MDS), as part of the new resident’s admission history. The oral health
history should include information about oral health beliefs, oral care practices and current
state of oral health, as perceived by the resident or his or her caregiver. A sample oral
hygiene history questionnaire has been developed by the RNAO and is included with this
document (see Appendix E).
4.2. Regular Oral Assessment
Nursing assessment of oral health should be done within 24 hours of admission, at least
quarterly thereafter, and whenever the resident, a family member or caregiver identifies a
change in oral health status. Ontario’s Halton Region Health Department has developed an
oral health assessment tool for this purpose.
Oral Health Assessment Tool
Using the Oral Health Assessment Tool
5. Oral Care Plan
All residents, including those who do not have natural teeth (with or without dentures), should
have an individualized oral care plan. The oral care plan should be reviewed and modified as
needed after each oral assessment. An example of an oral hygiene care plan and a guide to
interventions for residents in LTC are available from Ontario’s Halton Region Health
Department.
Oral Hygiene Care Plan for LTC
Dementia Reference Tool
15
6. Education of Staff
LTC facilities, in collaboration with dental health professionals, should implement continuing
education opportunities for nurses and personal support workers that include appropriate oral
health knowledge and skills training. Samples of training materials are provided in the resources
section.
RESOURCES
1. Oral Care Best Practices Sources
Oral Health: Nursing Assessment and Interventions Best Practice Guideline
This guideline, developed by the RNAO as part of its evidence-based Nursing Best Practice
Guidelines Program, focuses on specific vulnerable populations (those who need assistance to
meet their oral hygiene needs).
Oral Health: Nursing Assessment and Interventions Recommendations
This is a summary of the recommendations from the RNAO Oral Health Best Practice
Guideline.
Best Practices Approach to Oral Care in Long-Term Care Homes
These materials were developed by the Ontario’s Regional Geriatric Program central, one of
five geriatric regional programs in Ontario.
2. Training Resources
The following resources were developed by the Halton Oral Health Outreach Program of the
Halton Ontario Region Health Department. They are designed to assist in the education of staff
in LTC facilities.
• Basic Oral Care - K.I.S.S
• Dysphagia: Oral Health Care Tips for Individuals That Have Difficulty Swallowing
• Palliative End Stage Care
• Dementia Care
• Dry Mouth: Managing Xerostomia (Hypo-salivation)

16
• Diabetes: Managing Oral Care for the Elderly Diabetic
• Oral Pathology Basics: Common Mouth Sores in the Elderly
• Tooth Abscess: Recognizing a Tooth Abscess
• Cancer Care: Mucositis
• Denture Care
• Oral Health Products and Tips
3. Oral Care for Patients With Dementia – DVD
Oral Hygiene: Managing Oral Care for Residents with Responsive Behaviours – This
instructional 16-minute video/DVD was developed by the RNAO as part of the evidence-based
best practice guideline Oral Health: Nursing Assessments and Interventions. It is designed to
assist caregivers in providing proper oral care for patients with dementia and is available from
www.rnao.org. (Cost is $15. The material may be replicated in its entirety for educational
purposes only, with appropriate credit or citation.)
4. Oral Health Promotion Fact Sheets for LTC
These Oral Health Promotion Fact Sheets for Long-term Care were developed by the Health
Promotion Unit, Centre for Community Oral Health - Faculty of Dentistry, University of
Manitoba.
University of Manitoba’s Centre for Community Oral Health
5. Oral Health Educational Material for LTC
These Oral Health Educational Materials for Long-term Care were developed by the University
of British Columbia ELDERS (Elders Link with Dental Education, Research and Service)
group.
University of British Columbia ELDERS Group

Appendix A
Community Form PATIENT INFORMATION RECORD
Please bring to dental appointment
NAME: _____________________________________________Ƒ Dr. Ƒ Ms Ƒ Mrs. Ƒ Miss Ƒ Mr.
Male_____ Female_______
BIRTH DATE ____ / ____ / ____
YEAR MONTH DAY
ADDRESS: ________________________________________________________________
TELEPHONE. No. _______________ PHYSICIAN: ___________________________
CONTACT __________________________ Relationship___________________________
HOME: (
____)_____________________ BUSINESS: (____)_______________________
MEDICATION LIST
(Please list ALL medications, including non prescription drugs)
1. ________________________________________
2. _______________________________________
3. ________________________________________
4. ________________________________________
5. ________________________________________
6. ________________________________________
7. ________________________________________
8. ________________________________________
9.
ALLERGIES
:__________________________________________________
For patients on Warfarin (Coumadin): Most recent INR
Date:_______ Reading:__________
ADDITIONAL INFORMATION FOR PATIENTS WITH CAREGIVERS:
MOBILITY:
Does patient use: Wheelchair_____ Walker________
Able to transfer to dental chair:
Ƒ
NO
Ƒ
YES
Ƒ
with minimal assistance
Ƒ
with 2 persons assisting
COGNITIVE/SENSORY STATUS:
Alert ___ Mildly confused _____ Moderately confused ____ Advanced cognitive impairment ____
Hard of hearing
Ƒ
NO
Ƒ
YES mild ___ moderate ___ profound ___
Please answer the following questions:
REASON FOR VISIT________________________________________________________________
Last dental visit_____________________
Radiographs available__________________________
Optimal Health for Frail Older Adults
17

Optimal Health for Frail Older Adults
1
Appendix B
Hospital Facility PATIENT INFORMATION RECORD
Please fax to _________________________ prior to appointment date
NAME: _____________________________________________Ƒ Dr. Ƒ Ms Ƒ Mrs. Ƒ Miss Ƒ Mr.
Male_____ Female_______ BIRTH DATE ____ / ____ / ____
YEAR MONTH DAY
ADDRESS: _________________________________________
UNIT/FLOOR: _________ TELEPHONE. No. _________________
PHYSICIAN: _____________________ PRIMARY CARE NURSE: ________________________
SDM: _________________________________
HOME: (
____)____________ BUS: (____)_______________ CELL: (____)_______________
ALTERNATE CONTACT _______________________________
HOME: (
____)__________________ BUSINESS: (____)____________________
INSURANCE:
Ƒ NO Ƒ YES _____________________________________________
PERSON RESPONSIBLE FOR PAYMENT OF ACCOUNT: _________________________
ADDRESS:
REASON FOR REFERRAL/VISIT:
MEDICATION LIST (Please list ALL medications, including non prescription drugs OR attach MARS)
For patients on Warfarin (Coumadin): Most recent INR Date:_______ Reading:__________
ALLERGIES:
MOBILITY:
Does patient use: Wheelchair_____ Walker________
Able to transfer to dental chair:
Ƒ NO Ƒ YES Ƒ with minimal assistance Ƒ with 2 persons assisting
COGNITIVE/SENSORY STATUS:
Alert ___ Mildly confused _____ Moderately confused ____ Advanced cognitive impairment ____
Hard of hearing
Ƒ NO Ƒ YES mild ___ moderate ___ profound ___
Please answer the following questions:
1. Is patient in pain? Yes ___ No ____
2. Does patient have an acute infection? Yes ___ No ___If yes, describe location of pain/infection and
if pain is intermittent or constant, and duration of pain.
3. What treatment for pain relief/infection has been used?
18
Optimal Health for Frail Older Adults
1
.
.
.
.
.
.
.
.
.
.
Best Practices Approach to Oral Care in LTC Resource Kit March 2008
Oral Care Gap Analysis
Based on the RNAO Oral Health BPG Recommendations (2007).
Compare your LTC home’s practices, policies and procedures to those in the RNAO’s Oral Health
Best Practice Guideline.
Appendex C
Oral Care Gap Analysis
19

Optimal Health for Frail Older Adults
19
Best Practices Approach to Oral Care in LTC Resource Kit March 2008
Appendex C
Oral Care Gap Analysis
20
Optimal Health for Frail Older Adults
20
.
.
.
.
.
.
.
.
.
.
Best Practices Approach to Oral Care in LTC Resource Kit March 2008
Available for download on www.rgpc.ca
>> Long-Term Care Best Practices Resource Centre
Appendex C
Oral Care Gap Analysis
21
Optimal Health for Frail Older Adults
21
Appendex D
Sample LTC Oral Care Policy
Best Practices Approach to Oral Care in LTC Resource Kit March 2008
Oral Care
Policy
This is a SAMPLE LTC Oral Care policy and it can be used as a template.
LTC Home
SAMPLE ONLY- feel free to adapt to your LTC home
Nursing
Subject
Oral Care
POLICY:
1. An oral health history will be completed as part of the resident admission assessment and will
include oral hygiene beliefs, practices and current state of oral health.
2. Assessment of oral health will be included in all resident health assessments:
• Within 24 hours of admission
• At least quarterly and annually
• As oral health status changes
3. Residents’ oral health status will be assessed using the Oral Health Assessment Tool (OHAT)
for Long-Term Care.
• For LTC homes using MDS-RAI 2.0: complete Sections K and L , as necessary, complete
the OHAT to supplement the RAI with additional oral status information.
4. An individualized Oral Hygiene Care Plan (plan of care) will be determined and implemented
based on the completed oral assessment (OHAT), MDS Dental Care RAP, resident’s
preferences, functional ability, cognition and ability to cooperate and follow instructions.
5. Staff will provide, remind or cue oral care for residents at least twice daily. If possible, oral care
should be completed in the resident’s bathroom (i.e., due to the physical cues available).
6. Prior to initiating oral care, staff should review the oral hygiene care plan and be aware of the
resident’s cognitive status, their responsive behaviours, communication, sensory and functional
impairments, and dysphagia.
7. Encourage residents to be independent with oral care. Staff will complete any oral care that the
resident was not able to complete. Staff will provide or supervise the provision of oral care for
those residents at risk of aspiration.
8. Communicate with the resident at all times during oral care ensuring that the resident is aware
of the steps of the procedure and independent tasks required.
9. The “Approaches to Oral Care” tool can be used as a resource for staff in completing resident’s
oral care. Recommended interventions:
22

Optimal Health for Frail Older Adults
22
Appendex D
Sample LTC Oral Care Policy
.
.
.
.
.
.
.
.
.
.
Best Practices Approach to Oral Care in LTC Resource Kit March 2008 10
Never use toothpaste or mouth rinses with residents who have swallowing difficulties. Only
use water.
Never use lemon glycerine swabs with oral care.
The resident should be properly positioned to receive oral care.
For residents who are unable to keep their mouth open, use mouth propping devices
(ie. two toothbrush technique, wedges, etc.)
Use a toothbrush with a small head, soft bristles and a larger handle with a rubberized grip.
Use pea size amounts of toothpaste.
10. Interventions for care of dentures:
Never use denture tablets for soaking dentures of residents with dementia. The ingestion
of tablets/solution is serious. Vinegar/water solution can be used as an alternate (mix ½
water and ½ vinegar).
Remove dentures daily for at least three hours, for gums to rest.
Clean dentures with denture paste, denture brush and soak in cool water.
Brush the mouth tissues and tongue with soft bristle brush prior to applying the dentures.
Dentures should be thoroughly rinsed
11. Denture cups and toothbrushes will be labelled and replaced every 3 months and as required.
Replace toothbrushes after every oral infection.
12. The effectiveness of the oral care interventions will be evaluated at least quarterly. Additional
or alternate interventions will be added as necessary.
13. At the time of admission and throughout their stay, residents will have access to oral health
professionals including dentist, denturist and dental hygienist.
14. Based on the nursing assessment and in consultation with the resident and /or SDM, referrals
to an oral health professional (dentist, denturist, dental hygienist) will be made.
EDUCATION:
1. Orientation: New staff, Registered Nursing staff and Personal Support Workers / Health care
Aides (full and part-time) will receive oral hygiene care education and information during their
orientation.
2. Continuing Education: Staff education sessions regarding oral care hygiene will be provided
annually and additionally, as required.
QUALITY/ AUDITING MONITORING:
The LTCH Satisfaction Surveying process will include an annual evaluation of:
1. Residents’ satisfaction with oral hygiene care received
2. Family / SDM’s satisfaction with oral hygiene care provided.
23

Optimal Health for Frail Older Adults
23
Appendex D
Sample LTC Oral Care Policy
Best Practices Approach to Oral Care in LTC Resource Kit March 2008 11
Procedure
Denture Care
a) Introduction
• Plaque & tartar form on dentures just the same as they form on natural teeth
• Brush dentures (as you would natural teeth) at least twice daily
• Remove dentures daily for at least 3 hours for gums to rest, overnight is easiest
• Use a separate brush for any natural teeth
• Ask the resident to remove their dentures. Assist, if they can’t
• For upper dentures
• slide your index finger along the denture’s side then push gently
against the back of the denture to break the seal. Grasp it and remove
by rotating it. Grasp lower dentures at the front and rotate.
• For partial dentures
• place thumbnails over or under the clasps, apply pressure, being
careful to not bend the clasps and catch them on lips or gums.
b) Cleaning dentures:
• Wear gloves
• Line the sink with a towel. Fill it with some cool water just in case the dentures slip and
fall. Hot water can warp dentures.
• Rinse with cold water to remove food
• Scrub dentures using a denture brush and denture paste. Never use abrasive
cleansers or scouring powders
• Thoroughly brush all surfaces especially those that touch the gums. Rinse
well.
• At bedtime, place dentures in denture cup with cool water and vinegar (½ water and
½ vinegar)
• Only soaking them overnight with a cleansing table is not sufficient – it doesn’t clean
off the plaque
• NEVER use denture tablets for soaking dentures of residents with dementia -
ingestion of tablets/solution is serious
• Never use vinegar on dentures with any metal on them as this will cause the
metal to turn black.
24

Optimal Health for Frail Older Adults
24
Appendex D
Sample LTC Oral Care Policy
.
.
.
.
.
.
.
.
.
.
Best Practices Approach to Oral Care in LTC Resource Kit March 2008 12
Toothpastes
• Use pea-sized amounts of toothpaste, squeezing out a long strip of toothpaste is too
much
• Most toothpastes have a strong taste, many residents don’t like this, not appealing to
residents with Alzheimer’s Disease
• Foaming action of toothpaste increases saliva flow & will result in the resident wanting
to spit >> choke, gag
• DO NOT use toothpaste for residents who have dysphagia, who cannot swallow or
spit/rinse properly, have high level of dementia - there are oral cleansing gels available
Toothbrushes
o The best type of toothbrush to use for residents
is one with a small head, soft bristles, larger handle with rubberized grip
2-Toothbrush Technique:
For residents who bite down during care, consider using 2 toothbrushes – one to
prop the mouth open and one for cleansing
o Replace toothbrush:
• every 3 months or after an infection
Available for download on www.rgpc.ca
>> Long-Term Care Best Practices Resource Centre
25
Optimal Health for Frail Older Adults
25
Appendex E
Sample Oral Hygiene History
Oral Health: Nursing Assessment and Interventions
66
Appendix D: Oral Hygiene History –
Sample Questions
Please Note: These are suggested questions to assist in taking an oral hygiene history. It is not a validated
tool for the assessment of the person’s oral health history.
Admission Oral Hygiene History Sample Questions
Hygiene Beliefs:
Which statement best describes your beliefs regarding your teeth:
a) I expect that with proper care my teeth will last me a lifetime.
b) No big deal if I lose my teeth, most people do when they get older.
c) If I lose my teeth I can always get dentures.
Where on a scale would you place your oral health?
1 3 5
Not Important Somewhat Important Very Important
Personal Practices:
1. Are your teeth your natural teeth? Do you have dentures? Do you have crowns?
If the client has dentures: Do you have partial or full dentures? Do they fit properly?
How long have you had the ones you are currently using?
2. Are you having any difficulty doing your oral care?
3. How often do you brush your teeth in a day?
4. What type of toothbrush do you use?
5. What type of toothpaste do you use?
6. How often do you replace your toothbrush?
7. Do you use mouthwash?
8. Do you floss regularly?
9. Have you used tobacco products within the last six months? If so, how many cigarettes/cigars/pipes
do you currently smoke a day or how much chewing tobacco do you use?
10. Do you drink caffeinated beverages?
11. How often do you visit the dentist?
12. When was the last visit to the dentist?
13. Does going to the dentist upset you?
14. Do you have difficulty chewing or swallowing?
15. Is there anything else that you do to keep your mouth healthy?
Current State of Oral Health:
1. Are you currently experiencing any problems in your mouth?
2. Are your teeth sensitive to hot or cold?
3. When was your last visit to a dentist?
4. Are you currently taking any medications?
26
